Dr. Armin Delgado Salinas is a neurologist and specialist in pediatric neurophysiology. He currently leads the Neurophysiology Department at the National Essalud Hospital “Edgardo Rebagliati Martins,” where he conducts electroencephalography studies on neonates and children. His focus is on diagnosing neurological disorders through the evaluation of brain activity.
NN: Hello Dr. Armin Delgado, could you start by introducing yourself?
Dr. Armin Delgado: My name is Armin Delgado, and I am a neurologist. I am in charge of the neurophysiology department at the National Essalud Hospital Edgardo Rebagliati Martins, specifically in the pediatric area. In this unit, we conduct electroencephalography studies on neonates and children up to 14 years old.
NN: What are the main clinical indications for performing an EEG in neonates?
Dr. Armin Delgado: The main clinical indications for performing an electroencephalogram in neonates are to rule out epileptic processes or metabolic disorders that could affect the brain function of a newborn. It can also be used to determine gestational age and in hypothermia protocols. These are the three most clinically relevant areas.
NN: What specific electrophysiological differences are observed in neonatal EEGs compared to adults? How does this influence clinical interpretation?
Dr. Armin Delgado: The difference between a neonatal EEG and a non-pediatric one is significant. Starting with the fact that EEGs performed on neonates use what we call extracerebral electrodes. That is, we not only place electrodes on the brain but also on the eyes, chin, a respiratory band, and we record responses using what we call an electrocardiogram.
Why do we do this? Because, during the early neonatal period, it is often difficult to differentiate the baby’s state—whether they are awake, in active sleep, or in passive sleep. This differs from older children, such as those one or two years old, where we generally only place electrodes on the brain.
This has a direct clinical implication because the baseline tracing of the EEG, in terms of age-specific graphoelements, is very different in neonates or newborns.
The weekly differences set a standard for electrical maturity compared to what we see in children older than two months. Furthermore, global sleep classifications indicate that starting from two months of age, there is a resemblance to classifications used for older children or adults.
For this reason, in children under two months, we use a different classification. Having a tool like the electroencephalogram helps us, among other things, to evaluate what I previously mentioned: brain maturity.
NN: What are the main technical challenges you face when performing EEGs in neonates, and how do you overcome them?
Dr. Armin Delgado: Well, performing a neonatal electroencephalogram is genuinely difficult. Our nurse, who has been trained in this area for over 15 years, has always faced technical challenges. For us, interpreting a neonatal EEG is very different from a pediatric EEG, which represents a significant challenge.
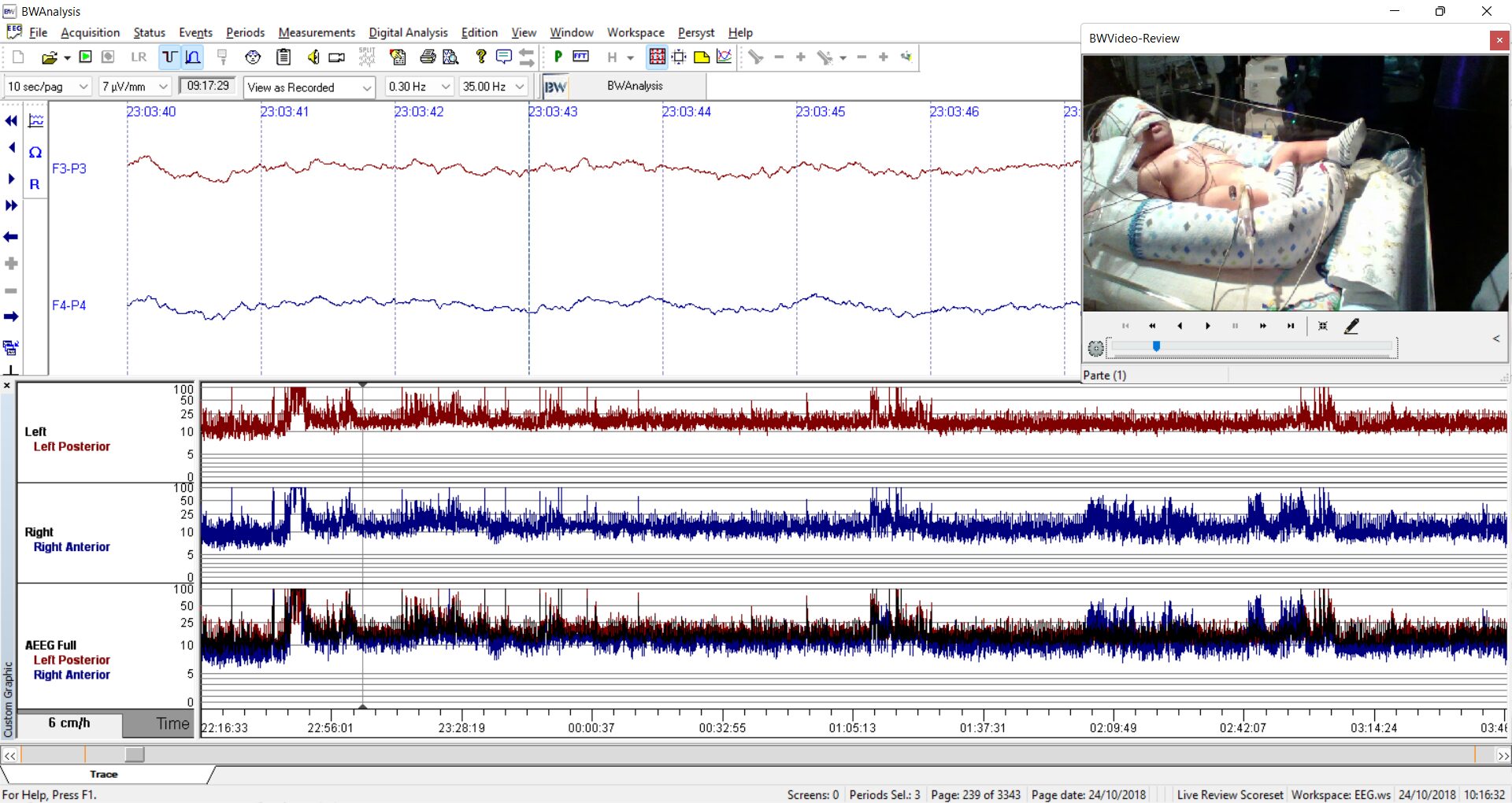
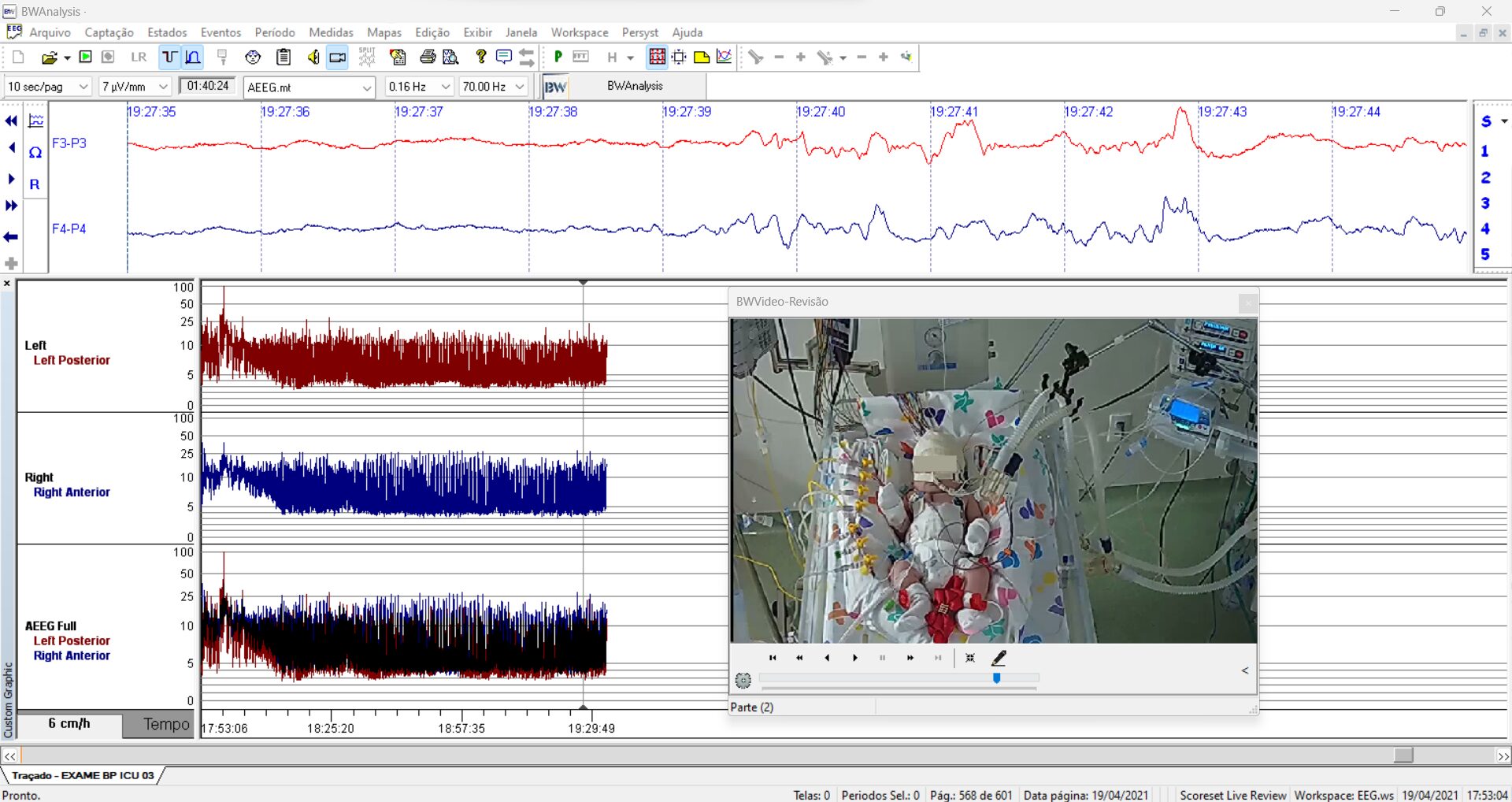
Usually, the babies we see are in complex areas like the pediatric ICU or neonatal unit, which are routinely surrounded by numerous electrical devices. This means the electrical field in these settings is challenging. The presence of numerous electrical fields generates noise or, colloquially, artifacts. These external interferences, which are not brain-originated, affect the signal tracings.
However, over the years, we have learned to manage these difficulties better. Besides thoroughly cleaning the scalp and using suitable materials, we have discovered that conducting studies with battery-operated equipment, instead of devices plugged into the wall, helps us obtain a more accurate tracing free from external electrical field influences.
In this sense, when we perform EEGs in pediatric or neonatal areas, we always aim to achieve a clean signal. The technical characteristics of the equipment we use have significantly contributed to minimizing or eliminating these external artifacts. We have also learned that distancing equipment from areas with high concentrations of electrical devices improves the quality of the recordings. For instance, in neonatal units with premature babies, where infants are often in incubators or connected to large devices, we have achieved better results by temporarily unplugging these devices for a few minutes.
With practice, we have also found certain filters helpful in reducing interference. Likewise, we minimize nearby movements, avoiding electrical devices or frequent personnel circulation around the recording area.
Additionally, we have learned to handle other interference sources, such as personal devices. For example, if a close relative (like a mother or father) is nearby, we ask them to completely turn off their cell phones because the electrical signal from these devices generates significant interference in the tracing.
In essence, we understand that recording a good neonatal EEG is a challenge, but through effort and experience, we have managed to obtain more accurate recordings that faithfully reflect brain waves.
NN: What pathological conditions are most frequently identified in neonatal EEGs? How do you determine the need for subsequent interventions?
Dr. Armin Delgado: Here in our neuropediatrics unit, where we have had the most support, it is mainly in the epileptic area. We have seen children who developed epilepsy from an early stage, and this has been one of the conditions that have most often required us to turn to this neurophysiological study.
The other area is metabolic issues, which also cause problems in newborns presenting conditions specific to their age, often associated with other conditions.
A third condition is neonatal asphyxia. These cases may be associated with the hypothermia protocol since decisions are needed to initiate this protocol. Hypoxia-related encephalopathy can be very severe and cause significant complications in the patient.
For this reason, the clinical implications of the electroencephalogram are crucial for initiating this protocol. As I mentioned, the hypothermia protocol has proven to be one of the treatments that can provide significant solutions for patients with this type of diagnosis, such as cerebral hypoxia.
NN: Do you recommend using Neurovirtual equipment for performing neonatal EEGs?
Dr. Armin Delgado: Yes, I would recommend Neurovirtual equipment. I have experience with these devices, and as I mentioned earlier, neonatal electroencephalographic electrodes always require the addition of extracerebral electrodes.
It is necessary to add electrodes at the ocular level, which we call electrooculogram; on the chin, corresponding to an electromyography; the respiratory band on the chest; oxygen saturation measurement; and also an electrocardiogram.
These additional setups can be used with Neurovirtual equipment, integrating them into the baseline electroencephalographic setup to obtain a complete recording of the neonatal condition.
NN: What are the best practices recommended for optimizing the quality of EEGs in neonates, considering the impact of environmental and physiological variables?
Dr. Armin Delgado: Based on my experience, having equipment in good condition, with adequate electrodes, and performing proper cleaning before the study is fundamental.
That is why it is important that, after each evaluation or electroencephalographic study, the materials used are left in suitable condition for the next study. It is also essential to have equipment with a fully charged battery and sufficient memory to conduct prolonged recordings, as we often need to extend the study beyond the recommended time, since neonates do not cooperate as easily as older children.
Sometimes, we ask them to sleep at a specific moment, and it may take a while for them to fall asleep, but they eventually cooperate. In other cases, with younger children, we only record during sleep. In neonates, it is more common for them to enter active sleep, which corresponds to future REM sleep, or quickly become alert, or even transition to the stage of non-REM sleep, which is future NREM sleep. Therefore, these recordings can be somewhat more variable.
International guidelines always suggest that neonatal EEGs should last at least 45 to 60 minutes. However, in our practice, we have noticed that neonatal studies often take longer. Why? Because we aim to differentiate whether there have been changes in wake/sleep stages and, above all, to observe the events that are part of the examination.
Therefore, managing these variables—both the maintenance of the equipment and the environment in which we work—is crucial. As I mentioned earlier, in practice, we face challenges because we bring such equipment to areas like ICUs, pediatric wards, or units requiring invasive or non-invasive ventilation, where additional electrical fields are also present.
To work in these areas, we need to have all preconditions well-prepared. In this way, we create a kind of checklist to avoid complications when using the appropriate materials.
NN: How do you use EEG findings to inform therapeutic decisions in neonates with epileptic seizures?
Dr. Armin Delgado: This goes hand in hand with teamwork. We try to ensure that the neurophysiology area is not an isolated department but one that works jointly with neonatology services. When the need arises, we coordinate in advance with the clinical teams—in this case, pediatricians and neonatologists—to address treatment decisions. This is particularly important when there are events that appear to be convulsive or ictal.
We receive information and take the equipment to the area, or, in some cases, the babies are brought to our unit, where we conduct complete video monitoring. This means that, in addition to the tracings and placement of both cerebral and extracerebral electrodes, we use video equipment for prolonged monitoring.
We can conduct video monitoring sessions lasting from 1 to 3 hours, with a maximum of up to 6 hours, accompanied by the neonatologist and the neurophysiologist in charge of the equipment. This way, while the recording is being performed, we evaluate events of a probable convulsive nature and make decisions based on the findings observed both in the recording and in clinical management.
As physicians, we understand that a clinical history is fundamental when making diagnostic and treatment decisions. In this case, when neonatal electroencephalograms become a challenging yet essential diagnostic tool, we use them in a practical way. As I mentioned, while performing the recording, we can make clear decisions.
Something we have learned over the years, and that we find crucial, is that the smaller the child, the faster the pathology manifests. It is interesting to note that sometimes a recording of one or five minutes, although brief, can be enough to directly show an abnormal electrical alteration.
When we perform longer recordings, we can quantify the percentage of this abnormality, providing us with valuable information about treatment prospects and, most importantly, prognosis.
NN: What are the key differences in the EEGs of preterm babies compared to full-term newborns? What are the clinical implications of these differences?
Dr. Armin Delgado: For all of us, physicians working in neurology and neurophysiology, viewing, interpreting, and analyzing a neonatal electroencephalogram is always a challenge. It is not straightforward. It is not like interpreting the EEG of a child older than two months, and even less so when dealing with a premature baby.
We know that, starting from 24 or 26 weeks of gestational age, the electroencephalogram is immature and progresses until reaching full maturity at term.
The concepts that have helped us and that we have learned over time include what we call the degree of continuity. As we observe the electrical tracing—without pauses or quiescence periods—we can see that the electroencephalogram is advancing appropriately.
What happens when we have a full-term baby, for example, at 38 or 39 weeks of gestation, and we find quiescence periods, or electrical quietness lasting more than six seconds? This does not indicate a good prognosis because the degree of continuity, in theory, should be practically constant, with no electrical gaps.
In preterm babies, we notice that as gestational age decreases, the periods of electrical quiescence (or gaps) become longer. However, understanding these electrical periods in relation to gestational age is essential to differentiate and interpret what is normal and what is not at that age.
It is crucial to recognize that, in the brain waves of a premature baby compared to a full-term newborn, the maturity or evolution of these waves is directly related to gestational age. Babies born at 38 or 39 weeks will have a nearly continuous tracing, reflecting cerebral maturity.
Conversely, in a premature baby, we must identify findings consistent with their gestational age, as this age group has unique characteristics that are well-defined. For example, bubble delta waves or brush delta waves are typical in babies between 32 and 34 weeks of gestational age, but this pattern disappears over time.
What happens if we find these waves in older babies, for example, at 40 or 42 weeks, when, in theory, they should no longer be present? This would indicate an electrical alteration related to gestational age. This could be associated not only with a potential pathology, such as epilepsy, but also with delayed brain maturity reflected in the EEG tracing.